Laparoscopic Parastomal Hernia Repair
Parastomal hernia is a common complication of stoma formation. Various surgical management options exist, of which laparoscopic mesh repair may offer shorter recovery times and reduced risk of recurrence.
Parastomal Hernia after Ileal Conduit
What is an ostomy or a stoma?
A stoma (ostomy) is a surgically created opening on the outer surface of the abdomen, through which urine or feces can be diverted into an external pouch following removal of part of the bowel or urinary system. Stomas may be temporary or permanent and are named according to the main conduit to which they are attached: Stomas involving the colon (large intestine) are termed colostomies, whilst stomas of the ileum (small intestine) are called ileostomies. Stomas of the urinary system, known as urostomies, are formed from a section of ileum that has been removed from the rest of the bowel, and to which the ureters (tubes that carry urine from the kidneys) are attached.
Why does a parastomal hernia occur?
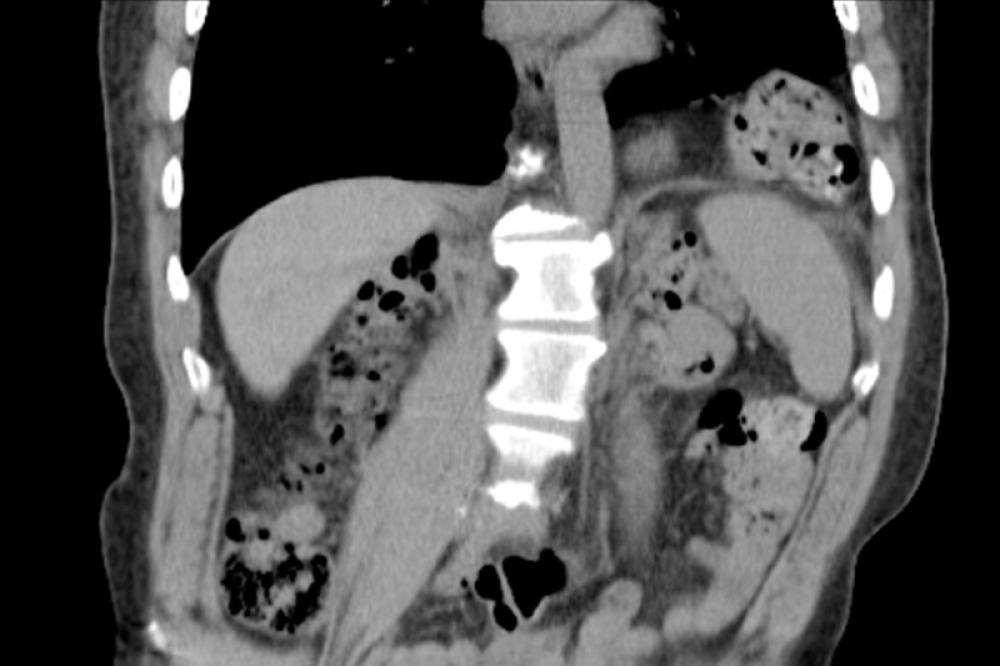
Parastomal hernia occurs when a weakness in the muscles of the abdominal wall allows a loop of bowel or other tissue to protrude out, resulting in a bulge or swelling around the stoma. Other symptoms include discomfort at the stoma site, abdominal distention, back pain, intermittent cramping, changes in stoma function and an increase in leakage due to poor fit of stomal appliances. Severe pain is not typical and warrants immediate medical assessment.
Contentiously, it has been argued that herniation is an almost inevitable consequence of stoma formation, since the procedure involves creation of an abdominal wall defect. Parastomal hernias can occur weeks or years after stoma surgery. Incidence figures vary widely throughout the literature, with medical imaging studies reporting higher rates of incidence than those based on clinical presentation. Colostomies are generally accepted to carry greater risk of herniation than ileostomies or urostomies. Other suggested risk factors include obesity, age, emergency stoma formation, postsurgical weight gain, infection of the stoma site, and increased intra-abdominal pressure (due to chronic coughing, heavy lifting, constipation, prostate enlargement).
The effects of stoma placement and construction upon parastomal hernia risk are currently unclear. Several studies have reported larger stoma trephine (opening) as a risk factor. Others have placed importance upon stoma location, suggesting that the trephine should pass through the rectus abdominus muscle so that it can provide internal support to the stomal conduit. There is evidence to suggest that prophylactic use of synthetic or biological surgical mesh to support the stoma trephine may reduce parastomal hernia risk. Postsurgical exercises designed to strengthen the abdominal muscles, and use of support belts during heavy lifting work have also been reported to reduce incidence of parastomal hernia.
When should fixing a parastomal hernia be considered?
Management of parastomal hernia may be conservative or surgical. Many parastomal hernias remain asymptomatic, and do not require treatment. Some people who experience discomfort find that it can be alleviated by wearing specially designed abdominal supports such as belts, girdles or support underwear. Where stoma dysfunction is present, modifying dietary habits or using a different type of appliance can help. However, some people may prefer surgical management. Indications for elective surgery include:
- Chronic pain or discomfort
- Changes in stoma function
- Peristomal skin irritation
- Leakage of stoma appliance
- Cosmetic issues
Rarely, a section of bowel may become trapped in the hernia, becoming perforated, obstructing the passage of waste or restricting blood supply to the affected tissue. This is a serious complication of parastomal hernia, requiring emergent surgery.
What are different types of parastomal hernia repair?
The three main categories of surgical parastomal hernia repair are direct fascial repair, mesh repair and stoma relocation. Smaller hernias may generally be repaired laparoscopically, whilst larger hernias, or complex cases (e.g. those involving intra-abdominal adhesions) may require laparotomy (open abdominal surgery). Laparoscopic repairs carry lower infection rates and reduced recovery time.
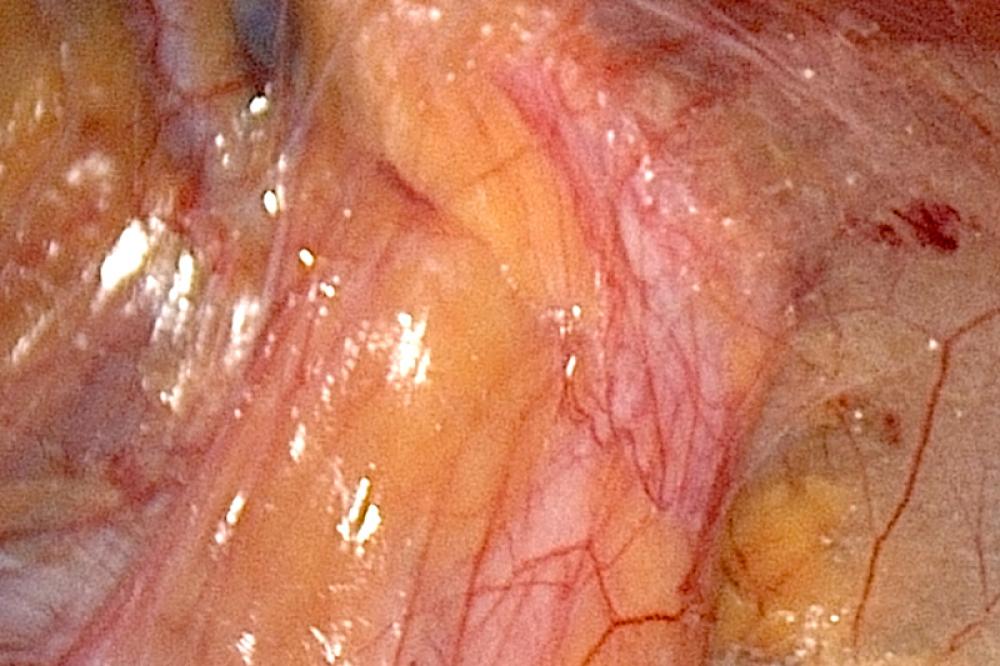
The fascia is a layer of soft, fibrous connective tissue that surrounds the abdominal and other muscles. During local fascial repair, an incision is made in the abdominal wall, the hernia contents are pushed back into the abdomen and the fascial defect is closed using sutures. This form of repair is associated with a high rate of recurrence and wound infection, so is not commonly indicated.
Relocating the stoma to a new position on the abdomen was previously the preferred approach to symptomatic parastomal hernia management. However, formation of a new stoma carries a high risk of recurrence relative to more recent forms of surgical management, particularly if the new stoma is located on the same side of the abdomen as the original stoma site.
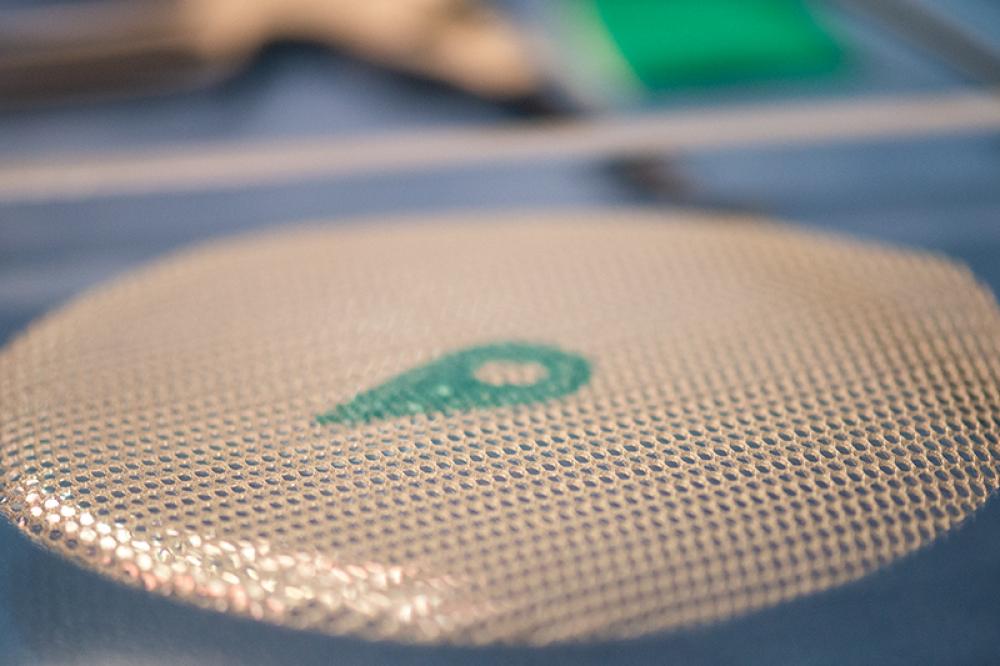
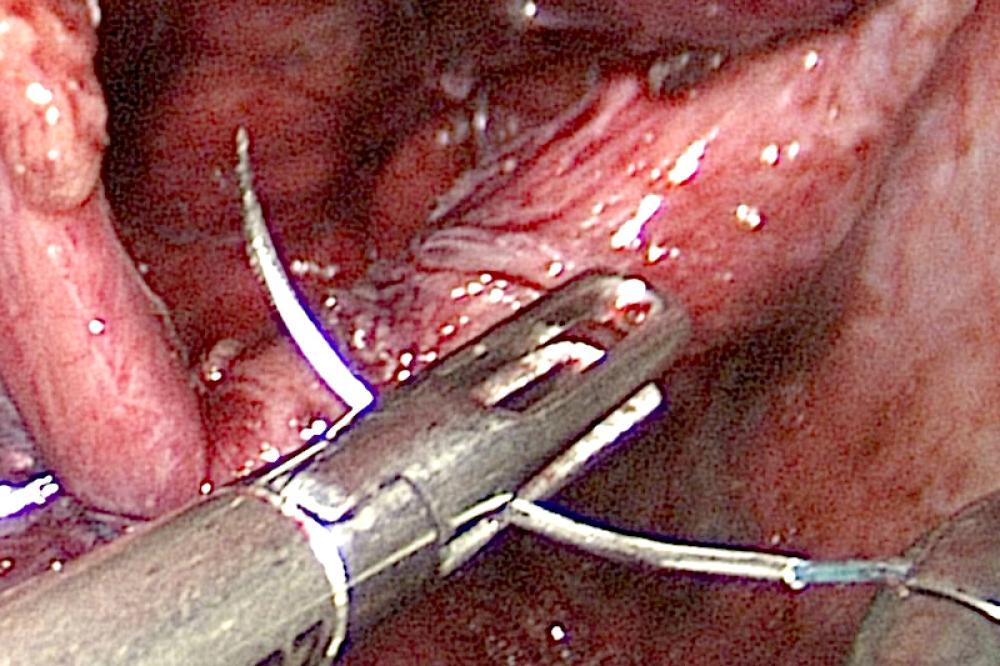
Mesh repairs utilize surgical mesh to close the defect or reinforce a sutured closure. Various different techniques may be employed. The onlay technique involves placing a piece of mesh with a central circular aperture directly onto the fascia around the stoma. In sublay placement, the mesh is located between the fascia and the muscle tissue. A slit may be created in the mesh so that it can be opened and placed around the bowel, or the bowel may be fully mobilized such that it can be pulled through the central aperture. Sutures are then used to secure the mesh to the bowel and abdominal wall.
Compared to onlay mesh placement, the sublay technique carries reduced risk of recurrence and of complications relating to contamination, but is associated with increased risk of adhesions and bowel obstruction.
Creating an aperture in the mesh may cause structural weakness and also complicates laparoscopic placement. The Sugarbaker technique is an alternative method utilizing an intact piece of mesh. The section of bowel that forms the stoma is lateralized such that it lies along the abdominal wall. A large piece of mesh is then placed over the stoma, covering the defect and forming a tunnel around the bowel, thus preventing other tissue from entering the stoma trephine. Recent studies indicate the Sugarbaker technique to be safe and associated with a low rate of recurrence.
PTFE (polytetrafluoroethylene) and polypropylene meshes are the types most commonly used for parastomal hernia repair. PTFE is softer and more pliable than polypropylene mesh, and is associated with reduced incidence of adhesions and bowel erosion. However, it has much smaller pores, which could harbor bacteria. It therefore carries increased risk of infection and is not recommended for use in an infected field, as may be present during emergent procedures. It is also subject to shrinkage and is unsupportive of tissue ingrowth. Biosynthetic materials, such as those made from human or porcine collagen, are increasingly being used in other forms of hernia repair and offer another alternative, but lack of long-term data means their impact upon reherniation rate is currently unclear.
What is the recover like after laparoscopic parastomal hernia repairs?
Course of recovery will depend upon various factors including general health and the type and complexity of procedure performed. Most people can expect to be mobile within 24 hours of surgery and able to resume most normal day to day activities within a few weeks. Lifting and carrying should be avoided for several months.
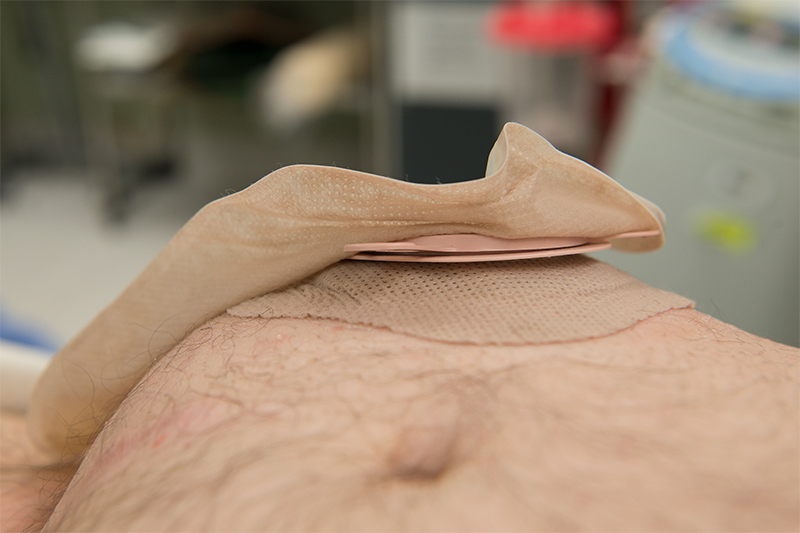
Use of an abdominal support garment or belt may be advised during recovery, and physiotherapy or a program of exercises designed to safely strengthen the abdominal muscles may be recommended to reduce the risk of recurrence.
There may be some temporary swelling and bruising around the stoma, which could affect the fit of stoma appliances. Postsurgical complications such as local infection are rare, but careful wound care is important and prophylactic antibiotics may be prescribed. Infrequently, some people can experience difficulty passing urine, and may need to wear a catheter for a few days.
In the longer term, a follow-up period of at least five years is often advocated as incidence of reherniation increases over time.
Recurrence of Parastomal Hernia and Prognosis
Recurrence is the main concern following surgical parastomal hernia repair. In addition to choice of procedure, factors thought to influence risk of reherniation are the same as those for primary parastomal hernia. In general terms, laparoscopic mesh repair may be associated with lower recurrence rates, and preventative steps such as weight management, abdominal exercises and regular use of supports during heavy lifting could help to further reduce risk. Biosynthetic materials may prove more effective than synthetic mesh, but long-term studies are currently lacking.