What is the gallbladder?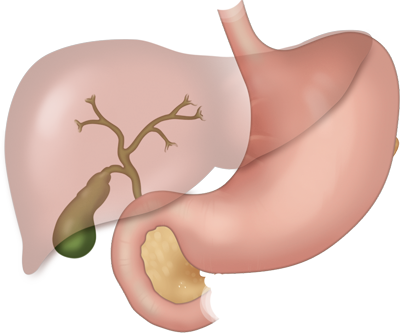
The gallbladder is located near the liver and it is a small pear-shaped organ that stores extra bile. Bile is made of water, cholesterol, biliary salts and biliary acids and is a substance that is required to dissolve fat during digestion. The liver produces about one liter of bile a day and the gallbladder serves as a small storage container for a small fraction of the bile produced daily. This extra bile is released by the gallbladder to aid in digestion during especially fatty meals.
Normally, the bile stays liquid, and does not form deposits. But, if the composition of the bile modifies, cholesterol crystals can form. They are likely to combine with biliary salts and pigments producing gallstones, which are yellow-greenish and of variable sizes, up to the size of a golf-ball.
Because the majority of gallstones produce no symptoms, they require no treatment. These "silent stones" are often discovered during routine medical checkups or exams for other illnesses and therefore classified as asymptomatic. A conservative or wait-and-see approach is recommended.
In some instances gallstones may cause mild discomfort to severe pain. This pain is classically located in the right-upper quadrant of the abdomen and made worse after eating fatty foods. If your physician determines that gallstones are likely the cause of your discomfort and must be removed then gallbladder surgery is typically required. Gallbladder surgery is one of the most common types of surgery in the United States.
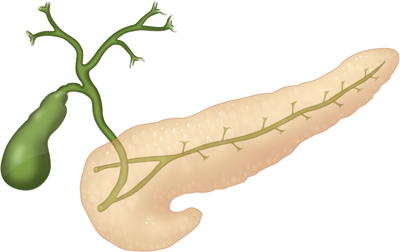
The gallbladder connects to the liver through a series of bile tubes. The liver produces a large amount of bile every day that travels through these tubes. A small amount is diverted into the gallbladder which then stores it until it is used as an extra reserve during fatty meals. The bile tubes connect with the tube system of the pancreas where they release their respective contents into the intestines, specifically the duodenum.
What lifestyle factors contribute to gallstones?
Family risk factors do contribute to gallstone formation. This means that if your mother and your father both needed gallbladder surgery during their lives then it is more likely that at some point in your future, you may also need a gallbladder operation. Some medications may possibly contribute to gallstone formation including cholesterol lowering drugs and hormone replacement therapy. Gallstones are more common in women.
Obesity, the diet associated with being over-weight as well as weight-loss also causes gallstones to develop. Therefore if you have an operation such as a gastric bypass, gastric sleeve or the Lap-Band and lose the excess weight that you are hoping to lose, then there is a good chance you may require gallbladder surgery in the future. This increased risk does not mean that you must have your gallbladder removed during a weight-loss operation. Typically gallbladder surgery is only performed at the same time as weight-loss surgery if you already have both gallstones and a history of being bothered by them.
What is laparoscopic cholecystectomy?
The Critical View
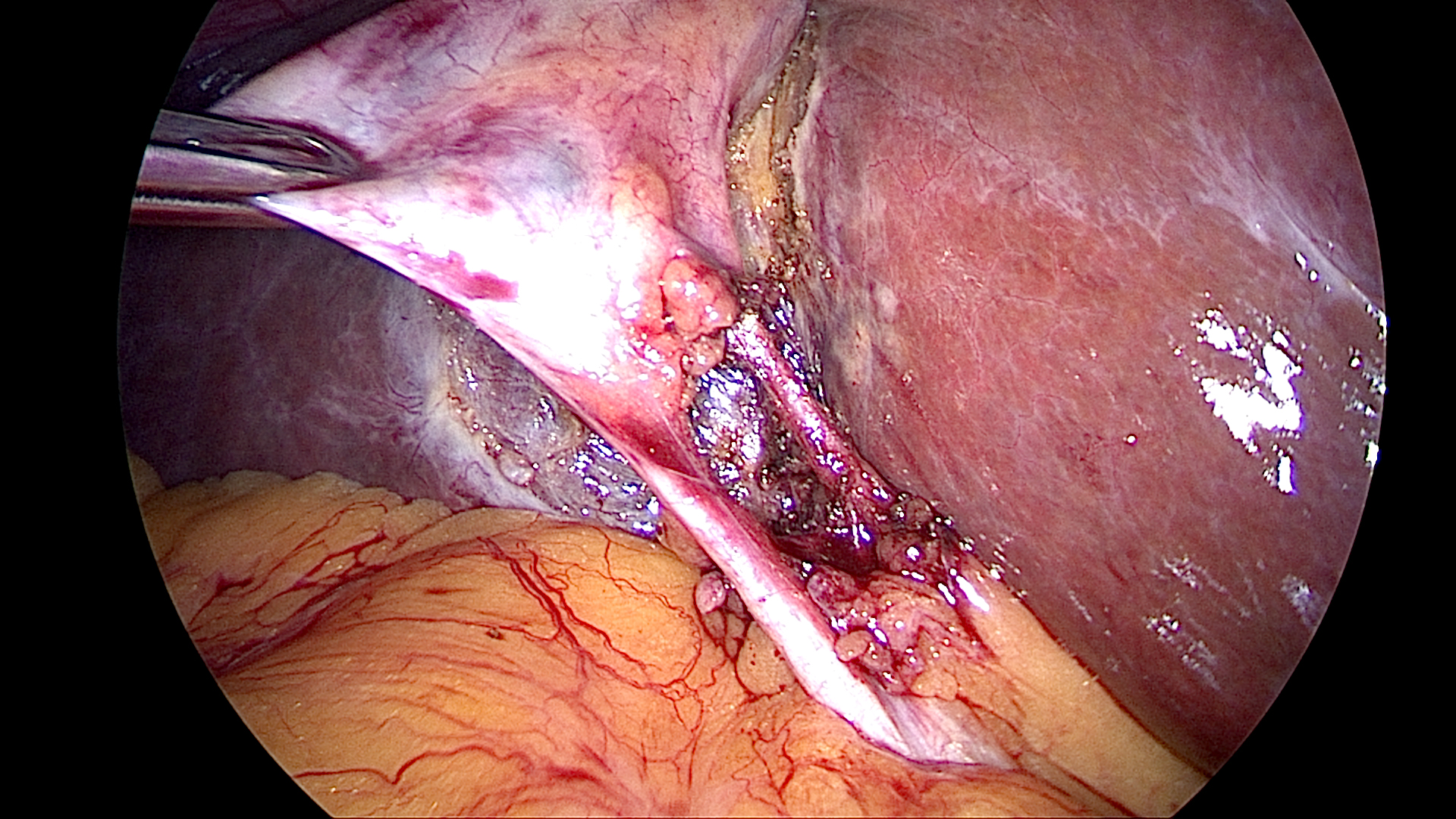
Gallbladder surgery when performed through the small cuts and a camera is called laparoscopic cholecystectomy.Removing the gallbladder is the preferred treatment for the majority of people who have gallstones that cause symptoms. Laparoscopic cholecystectomy requires several small incisions in the abdomen to allow the insertion of surgical instruments and a small video camera. After the initial incisions, the surgeon will use carbon dioxide to inflate the abdominal cavity. The camera sends a magnified image from inside the body to a video monitor, giving the surgeon a close-up view of the organs and tissues. The surgeon watches the monitor and performs the operation by manipulating the surgical instruments through separate small incisions.
The gallbladder is identified and carefully dissected free from its attachments under the liver. One of the most important portions of the procedure is the identification of Calot's Triangle. Calot’s triangle is an anatomic area bounded by the liver, cystic duct, and common hepatic duct. The cystic duct and the cystic artery are identified, clipped with tiny titanium clips and cut. The gallbladder is then separated from the liver bed and removed through one of the small incisions.
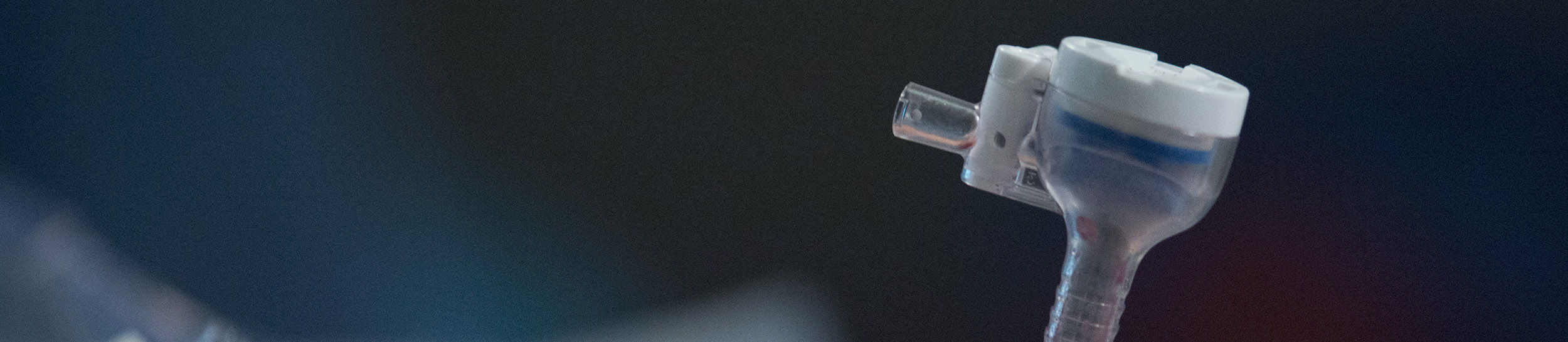
What tools are used for laparoscopic cholecystectomy?
A laparoscope is a small, thin tube that is attached to a video camera and placed into your body through a tiny cut. The surgeon can then see the gallbladder on a television screen and do the surgery with tools inserted in three other small cuts made in the right upper part of your abdomen. Only small incisions are required. The video camera then produces a magnified view on a television monitor of the inside of your abdomen allowing a very detailed view. A number of other laparoscopic instruments are typically used. The gallbladder is then removed through one of the small incisions.
Are there any benefits of laparoscopic cholecystectomy compared with open cholecystectomy?
Surgery to remove the gallbladder with a laparoscope does not require that the muscles of your abdomen be cut in the same manner as as they are in open surgery. With laparoscopic cholecystectomy, you may return to work sooner, have less pain after surgery, and have a shorter hospital stay and a shorter recovery time. Although there are more than one incisions, each incision is much smaller than the typical open incision which makes recovery much quicker.
Most laparoscopic cholecystectomy procedures are performed as an outpatient surgery meaning that you go home the same day as the operation and recover in the comfort of your home.
Is there any reason why I wouldn't be able to have a laparoscopic cholecystectomy?
If you have previously had surgery in the area of your gallbladder, if you tend to bleed a lot or if you have any problem that would make it hard for your doctor to see your gallbladder, an open surgery may be better for you. Your doctor will decide which type of surgery is best for you.
What are the complications of laparoscopic cholecystectomy?
Complications may include bleeding, infection and injury to the duct (tube) that carries bile from your gallbladder to your stomach. Also during laparoscopic cholecystectomy, the intestines or major blood vessels may be injured when the instruments are inserted into the abdomen. All of these complications are rare but still possible when performed by a laparoscopic surgeon.
What other procedures may be required?
If you have stones in the bile duct as well as your gallbladder, you may require removal of both the duct stones and your gallbladder. In some cases it is best to remove the stones in the bile duct before your operation using an endoscope. If you look at the image to the right, you can see that the stomach and intestines provide a route to get directly to the bile tubes without making cuts on the wall of the abdomen.
The procedure is called an endoscopic retrograde cholangiopancreatography (ERCP) and consists of a scope that is inserted through the mouth, down the digestive tract and then used to instrument the bile tubes from inside the intestines. If you have ERCP, your gallbladder may be removed at a later date or during the same hospitalization. Often, a cutting instrument is inserted through the endoscope, and the entrance of the bile duct is enlarged so the stone can pass through it. The same procedure may be used to remove a stone from a blocked pancreatic duct.
Are there long term effects after gallbladder removal?
Your liver will continue to produce enough bile to digest a normal diet after you have surgery. Please remember the liver produces over one liter of bile a day therefore it is unlikely that the small amount that was stored by the gallbladder will play a noticeable difference in digestion. You may notice you're having more bowel movements than usual and that their consistency is less solid. These symptoms usually lessen over time. It is normal to have a self-limited change in digestive habits that is unrelated to your type of operation and will improve over time. Some patients however find that diarrhea remains a problem, and a ‘heart-healthy’ diet or one that is low in rich, fatty foods will usually alleviate the problem.