What is Laparoscopic Surgery?
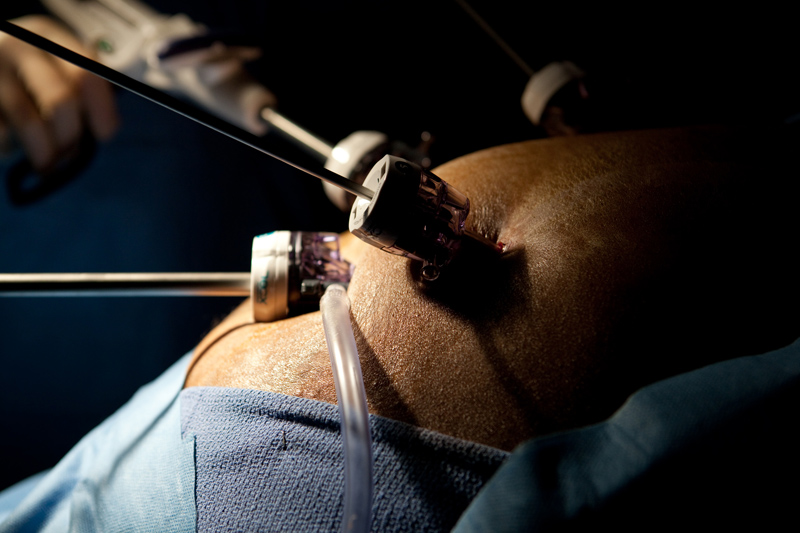
Today, laparoscopic surgery is a widely accepted surgical technique that uses small incisions and long pencil-like instruments to perform operations with a camera. As the incisions are much smaller than their open counterparts, recovery is faster and post-operative pain is typically less. Procedures such as hernia repairs, gastric bypass, bowel resection, and organ removal are now routinely carried out laparoscopically.
Minimizing Physiological Stress
Laparoscopic surgery has successfully replaced open surgery as the preferred treatment option for issues such as bariatric surgery and >gallbladder removal. In fact this surgery can now be performed as an outpatient operation. The treatment of gastroesophageal reflux disease is now carried out using minimally invasive techniques. Laparoscopic fundoplication offers the advantage of faster recovery and quicker return to oral ingestion of food. Laparoscopic surgery for weight loss has caught on in a big way. Laparoscopy has advanced sufficiently to the extent that it can be repeated for a patient who has undergone a previous laparoscopic operation. However, care needs to be taken than organs do not get injured and to this end the entry site may have to be different and an alternate entry technique may have to be used. The risk to benefit ratio of laparoscopic surgery is improving continuously in favor of benefits.
Historical Perspective for Minimally Invasive Surgery
There is general consensus amongst medical historians that the first credibly recorded instances of endoscopy can be credited to the Arabian physician Albukasim (936-1013 A.D). Seven more centuries were to pass before any further developments in endoscopy. In 1805, physician Phillip Bozzini used an illuminated light chamber, a tube, and mirrors for reflection in order to explore the human urethra. He was able to view the urinary bladder and to visualize stones and neoplasms.
Georg Kelling of Dresden, in present-day Germany, first used laparoscopes to view the peritoneal cavities of live dogs. Stockholm - born physician Hans Christian Jakobaeus was the first person to make use of a laparoscope on multiple human patients. He viewed different pathologies and he described conditions such as cirrhosis of the liver, metastatic cancer, and tuberculosis peritonitis.
The growth of laparoscopy was dependent on developments in sources of light that did not cause burns and lenses that magnified and increased the field of view. For example, in 1929, the introduction of a new lens system that permitted oblique (135°) viewing helped popularize laparoscopy in Europe. The advent of the dual trocar technique at around the same time gave a further fillip to diagnostic laparoscopy. The method enabled surgeons to both visualize the abdominal cavity and simultaneously to pass instruments into the cavities.
Optics and Laparoscopy
Advances in photography, optics, lighting, and access to the abdominal cavity have defined the development of modern laparoscopy as we know it today. The technique of "cold light" fiberglass illumination introduced by a team of French scientists in 1952 improved safety by eliminating the risk of intraperitoneal burns and electrical faults that took place when using intra-abdominal sources of light. The “cold light” came from an intense proximal light source outside of the abdominal cavity along a
Light Source
quartz rod to the distal end of an endoscope and it was intense enough to permit photographs to be taken. The advent of flexible fiber-optic instruments can be traced to this development. The 60s and 70s saw gynecologic practitioners making wide use of laparoscopic techniques. German engineer and gynecologist Kurt Semm is credited with having contributed the maximum to developments in interventional minimally invasive surgical technique. An automatic insufflation device designed by Dr. Semm in 1977 enabled surgeons to monitor both gas flow and intra-abdominal pressure.
Dr. Semm also developed techniques for knot tying and developed instruments that could execute the required maneuvers. He helped popularize procedures such as laparoscopic lysis of omental adhesions, bowel suturing, and tumor biopsy and staging. In 1981, Dr. Semm performed the first laparoscopic appendectomy.
How Have Visual Tubes Evolved?
Laparoscopic visual tools have evolved from endoscopy of which there is documented evidence that it was used as far back as 1806 to examine the canals and cavities of the human body. The first attempt at laparoscopic examination of the peritoneal cavity was carried out in 1901 and the procedure was termed “Celioscopy.”
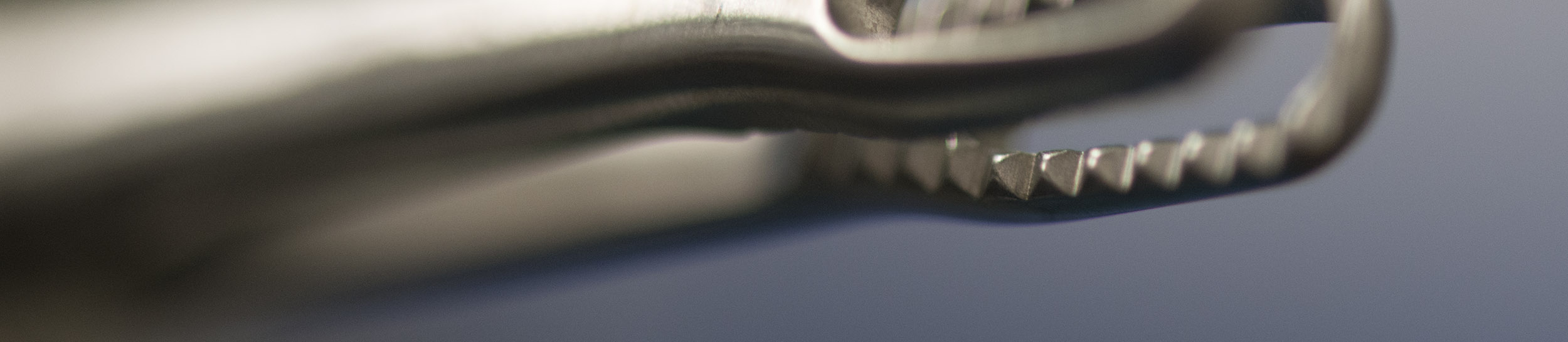
The Laparoscope as an Instrument

Laparoscopic techniques continued to develop and by 1930s, doctors were performing diagnostic biopsies of abdominal organs under direct visualization. The seventies saw laparoscopic techniques being commonly used by gynecologists. However, its spread in general surgical practice was limited because it did not facilitate complex surgical procedures because of the limited field of view and the fact that the surgeon’s hands were occupied in holding the laparoscope.
Thus, the year 1986 marks a watershed event in the evolution of laparoscopic surgery because it was in this year that the video computer chip was developed. This development enabled surgeons to project magnified images onto television screens and it paved the way for newer and more complex applications of laparoscopy. We can consider the year 1987 to be the year which truly heralded the arrival of laparoscopic surgery. This is because it was in this year that the first laparoscopic cholecystectomy or gallbladder removal was first performed.
Surgical Dogma and Laparoscopy
However in general surgeons were loath to accept laparoscopy as a genuinely useful form of surgery that needed further investigation and support. The reasons for this are not very clear but not having a clear field of vision during laparoscopy and surgical dogma that had existed for centuries are some of the reasons that slowed down the acceptance of this surgical technique.
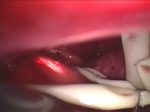
Limitation of Depth of Field and 2D View
Also, one of the chief hindrances to the development of laparoscopic surgeries is that unlike open surgeries the field available to the surgeon is two dimensional. This makes it difficult to acquire a perception of the depth and the surgeon has to proceed with extreme caution. The issue can be further compounded if there is a lack of illumination and vision is restricted.
Visualization
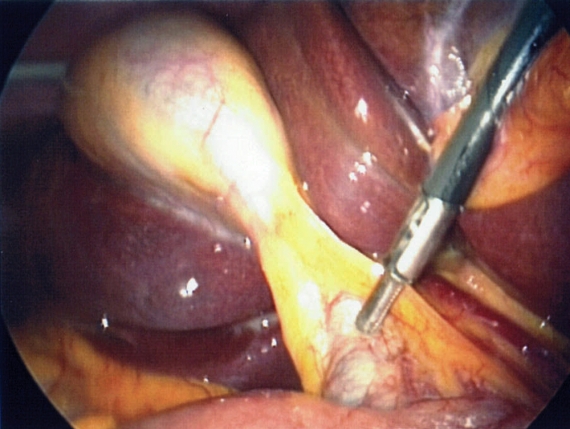
Internal bleeding due to errors in depth perception can also be hard to control. In the late eighties and early 1990s, gynecology was performing laparoscopy on a basis more common than general surgery. However, in 1987 a laparoscopically performed cholecystectomy (gall bladder removal) gained much approval and by 1992 more than half of the over one-half million cholecystectomies done in the United States were being performed laparoscopically.
These were the early surgical experiences with laparoscopy that helped surgeons understand and appreciate the potential benefits of laparoscopy such as a reduction in hemorrhaging so that the need for blood transfusion is reduced; incisions are smaller so that recovery time is short and there is less post-operative scarring; less pain so that less pain medication is required; less chance of internal organs being exposed to contaminants.
Laparoscopic Suturing