How Does a Gastric Bypass Change Dieting and Help Weight Loss?
Most people who opt for a gastric bypass procedure are aware that it is generally not reversible. There are major changes to the digestive system, changes that make this approach to bariatric surgery very effective in significant weight loss. At the same time, a gastric bypass is more than a surgical procedure; it is also part of a lifestyle change. It’s tempting to think of the surgery as doing the heavy-lifting in terms of losing weight. It’s certainly an important and possibly necessary component of a weight loss program, but in the long run, the digestive system changes should be just a part of a new digestive regime. In a sense, a gastric bypass is just a tool, something to help you with a lifelong diet. It’s important to understand how to use this tool to the best of your ability.
What changes happen to your digestive system with a gastric bypass?
Consider that your digestive system begins in the mouth (some would say it actually begins on the dinner plate). When you eat or drink the materials mix with salivary juices in the mouth, which begin the chemical breakdown that eventually will remove nutrients and energy calories for your body. Chewing food is (or should be) an important part of preparing food for digestive. It’s the only time your body provides you with a conscious and mechanical means of breaking up larger pieces of food – the rest of the digestive process occurs automatically. Chewing is especially important for people with a gastric bypass because there is so little room in the stomach that large chunks of food might cause a serious problem.
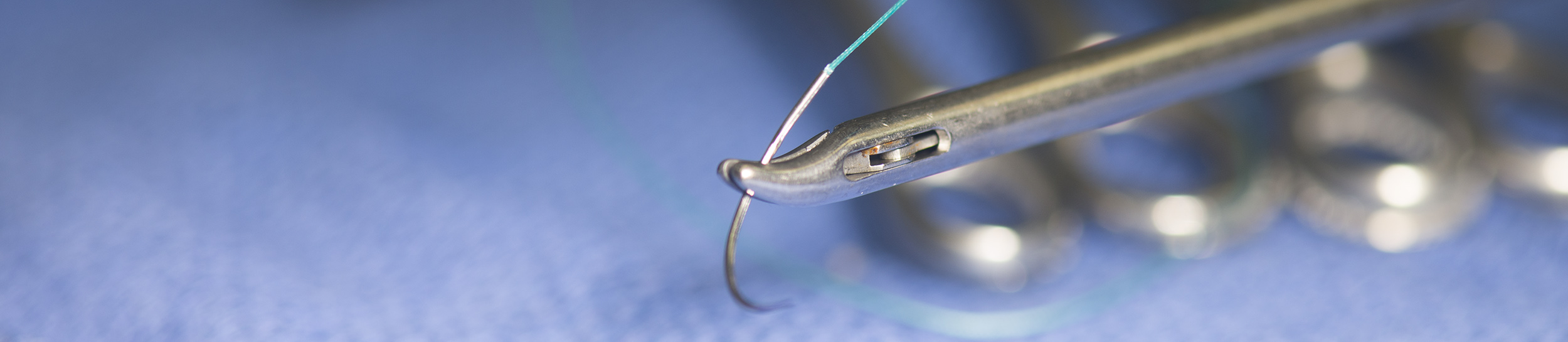
In the most common gastric bypass procedure, the Roux-en-Y (roo-en-Y), the surgeon creates a pocket at the top of the stomach by either suturing or stapling and thereby sealing off the lower stomach so that food no longer passes through it. What’s left of the stomach is approximately the size of a walnut or small egg and can hold only about 1 or 2 ounces of food or drink. Compare this to a typical normal stomach, which can hold roughly 6 cups (48 ounces) or 3 lbs. of food. Obviously, the restricted stomach means that very little food can be eaten at one time and the food coming into the stomach should be well masticated (chewed and mixed with saliva).
The drastically downsized stomach is one reason that a gastric bypass is effective in helping weight loss. The other aspect is the ‘shortcut’ past the upper portion of the intestines. Part of the Roux-en-Y procedure separates the uppermost portion of the intestine, the duodenum, from the middle portion, the jejunum. After separation, the surgeon extends and attaches the jejunum to the new stomach pouch. The duodenum, which is still connected the lower stomach, is attached further down on the jejunum – forming the “Y” of the procedure.
The reattachment of the duodenum allows for relatively normal physical operation of the remaining stomach (though without food) and especially for the flow of gastric juices coming from the liver, gall bladder and pancreas.
How to manage your digestion and make the most of a gastric bypass
After a gastric bypass, all patients are carefully instructed in what to eat and how to eat. The point is not only to protect the changed digestive system, but for the patient to take control over their diet, eating habits, exercise and other lifestyle choices. While the bypass makes a huge contribution to weight loss, the full program requires the active participation of the patient. For example, when to eat and how much to eat needs to be disciplined.
The standard advice is to eat more meals, around six times a day, but eating far less at each meal. Of course, with the very small stomach pouch of a gastric bypass, it’s not very difficult to eat too much too fast. Most people develop a chewing and swallowing rhythm so that they don’t pass too much food or drink to the stomach at one time. If done right, the slower pace allows for a feeling of fullness to develop, which becomes an automatic limitation on the desire to eat.
In a small percentage of people, the type of food they eat and the wrong eating habits may cause what’s called gastric dumping. In this disorder, food passes too quickly from the gastric pouch into the intestines. Overloading the upper intestine (duodenum in this case) may cause nausea, cramping, diarrhea, dizziness and fatigue. It’s most common with the Roux-en-Y form of gastric bypass. The first line of treatment is to eat meals low in carbohydrates, avoid simple sugars, and drink liquids between meals, not with them.
Another aspect of eating with a gastric bypass is mixing food and liquid. The general recommendation is that you avoid doing both at the same time. For example, most physicians recommend that you avoid drinking for about 30 minutes before eating, and wait at least an hour after eating before you drink again. These restrictions on drinking while eating are not arbitrary. It’s all too easy to “wash through” the food you eat by taking on liquids. When that happens, the tiny stomach pouch doesn’t have enough time to begin the digestive process. Often the food simply washes directly into the intestine (which in the gastric bypass means into the small intestine). The problem with this is simple – your body doesn’t register a full stomach and it’s very easy to overeat. You can eat so many ‘pouchfuls’ that, in fact, you don’t lose weight.
How a gastric bypass affects what foods to avoid or eat with caution
Post-operation, the diet is typically all-liquid for several weeks and then only soft or mashed foods until the post-surgical swelling in the digestive system heals. Thereafter, the small size of the gastric pouch (though it will stretch some over the months) and the reduced digestive capacity make it necessary to choose foods with some care. Potentially long term problematic foods include, seeds, popcorn, and some nuts. These foods food may be difficult to digest. Certain foods may expand in the gastric pouch and temporarily block your connection to the intestines or chronically cause pouch dilatation. Dried fruit may expand in the gastric pouch. Soft drinks with carbonation are not only bad for any diet (too much sugar) but the gas expansion effect of carbonation can be a real pain in the stomach pouch. Breads are high in carbohydrates. The difference between white bread and cake is not always so different from a nutritional perspective. Bread may throw off your glycemic index and may also be prone to expand in the pouch. From this list, it’s obvious that the cautionary for foods include – anything difficult to digest, foods that might block the gastric pouch exit, any food with sharp edges, and food or drink that has a tendency to expand in the stomach. You’ll probably develop a personally relevant list of foods to avoid or eat differently in consultation with your doctor, a nutritionist – and through experience.
A gastric bypass may change the intestinal biome
Over the last decade or so, a great deal of research has led to a reappraisal of the vastly complex ecosystem of bacteria that live in the human intestines. What’s now called the intestinal microbiome is the home to trillions of microbes, most of which are harmless or more to the point, essential for the digestive process. When the digestive system is significantly altered through a bypass, there is usually a corresponding significant change in the bacterial composition of the microbiome.
The gastric bypass actually provided scientists with an intriguing tip-off about the relationship between a changing digestive system, weight loss and type 2 diabetes. One very important reason for resorting to bariatric surgery is to halt or forestall the progression of type 2 diabetes – the type closely associated with obesity. However, doctors noticed that following a gastric bypass procedure, people with type 2 diabetes experienced an almost immediate improvement – long before they had a significant weight loss. There was speculation that the operation changed the hormonal balance in digestion and people simply did not want to eat as much or eat foods that encouraged diabetes. However, plausible research suggested that it may be due to a change in the bacteria of the microbiome.
In the last few years, a number of studies seem to indicate there is a beneficial change in the microbiome, that in fact, the types of bacteria that survive after a bypass operation make a significant contribution to weight loss. There is even evidence (in mice) that artificially increasing the population of certain bacteria can, by itself, induce weight loss. This is an area of research just beginning to enter the phase of clinical trials with human beings. It’s too early to identify the specifics of intestinal bacteria or whether there are also negative side effects. However, people with a gastric bypass could do well to stay abreast of new research in this area.
Changes in the absorption of food nutrients
The “bypass” in gastric bypass surgery means that the entire nutrient absorption normally taking place in the upper intestines, in the duodenum, no longer happens. In effect, this, in theory, reduces the ability to absorb nutrients and calories from food. Absorbing fewer calories makes it easier to lose weight.
Because the duodenum is very active in the absorption of vitamins and minerals, bypassing this section of the intestines can lead to deficiencies. Most common are vitamin B12, folate, zinc, iron, copper, calcium and vitamin D. These are all important in various physical process and deficiencies can lead to serious complications.
The abbreviated stomach also plays a role in some of these deficiencies. For example, vitamin B12, which is important in the growth and replication of cells and the functioning of the nervous system, needs the acid found in the stomach to begin the breakdown process that prepares it for absorption. It also needs the duodenum to bind it to specific proteins so it can be absorbed in the ileum (middle portion of the intestine). The combination of reduced stomach acid (most of which is produced in the lower stomach) and the bypass of the duodenum often leads to a vitamin B12 deficiency.
Sometimes the deficiencies have subtle digestive origins, for example, many people get their calcium in supplements of calcium carbonate (or from eating green vegetables such as broccoli). Calcium carbonate, which makes up most of eggshells and shrimp casings, needs stomach acids to break down into a form that can be absorbed by the intestines. With a very small stomach pouch, the calcium isn’t exposed to stomach acid long enough to properly break down, which can mean a lack of absorption and eventually a calcium deficiency.
The way around the digestive deficiencies is to take supplements and adjust the diet. Since there is wide variation in the way individual’s digestive systems react to the bypass surgery, doctors monitor the levels of key vitamins and minerals so they can prescribe supplements as needed.
Occasionally a gastric bypass may cause problems
The gastric bypass is a very common and typically safe procedures, especially when performed by laparoscopic methods. However, with any procedure that alters the digestive system, it is possible to have complications. Because the gastric bypass procedure involves several cuts and connections (anastomosis) there is always the possibility for leakage of fluids from the stomach or intestines. The same lines of connection may become infected, form scar tissue or at worst, ulcerate. Any of these developments may require a new surgery.
In addition to the physical complications associated with bypass surgery, there are complications in the digestive process as well. As mentioned before, vitamin and mineral deficiency may be common and relatively simple to treat. There are other nutritional effects that are more complicated, such as protein shortages (slightly different from a vitamin deficiency); this is a case where because of the bypass it’s not possible to absorb enough protein. While this may seem ironic, in some cases a calorie deficiency can occur, meaning that weight-loss can become excessive.
Finally, there’s one unpredictable effect of a gastric bypass that may develop; after about 18 months, the weight loss stabilizes or even reverses. Doctors aren’t sure why this happens, it may be different causes in different people, but here are some of the possible reasons:
- It may happen with a pattern of eating too much or the wrong foods and stretching the gastric pouch to accommodate much more food.
- For similar reasons, it might be a gradual enlarging of the intestine, which allows food to pass more quickly.
- While this may seem strange, it is possible for the intestine attached to the stomach to stretch until it becomes like a second pouch, holding more food.
- The intestinal biome adjusts until it re-establishes a bacterial content as it was before surgery.
Considering the risks, which tend to run less than 1-2% of all patients, gastric bypass methods are among the best for producing significant weight loss with few side effects and complications. While the irreversible surgery and the requirements for a careful digestive lifestyle call for life-long attention, the reduction in weight – going from obese to near normal – has so many health related benefits, the gastric bypass remains among the most popular of the bariatric procedures.