Laparoscopic Ventral and Incisional Hernia Repair
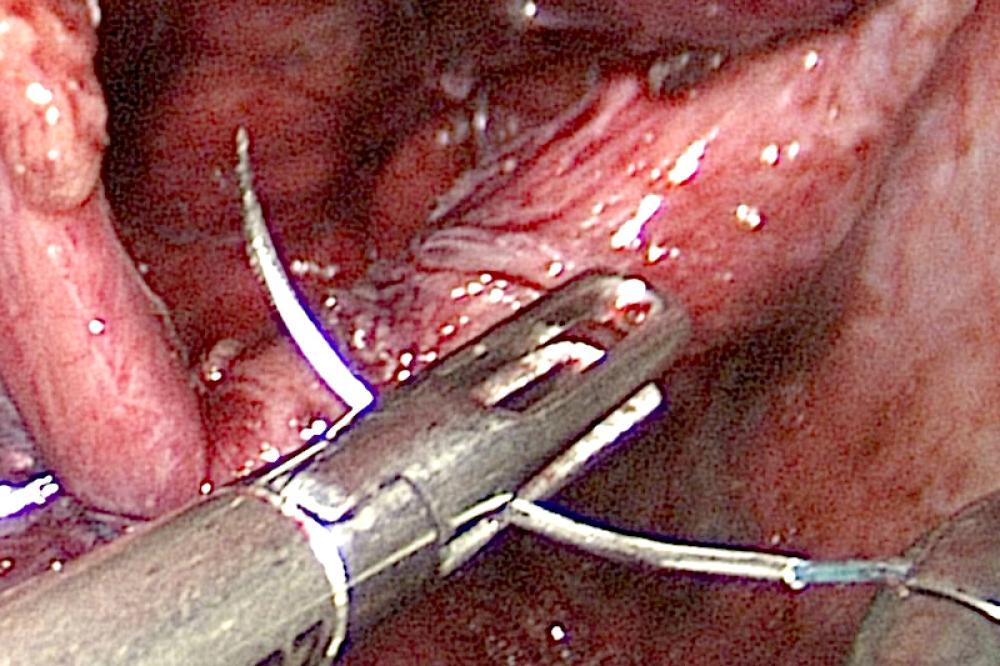
Trapped Intestine
Your abdominal wall has many layers and functions. Although some people think that the abdominal wall musculature is only used when performing a sit-up, the abdomen is actually an integral part of your core strength. Your abdominal muscles help every time you take a breath, laugh, or stand up straight.
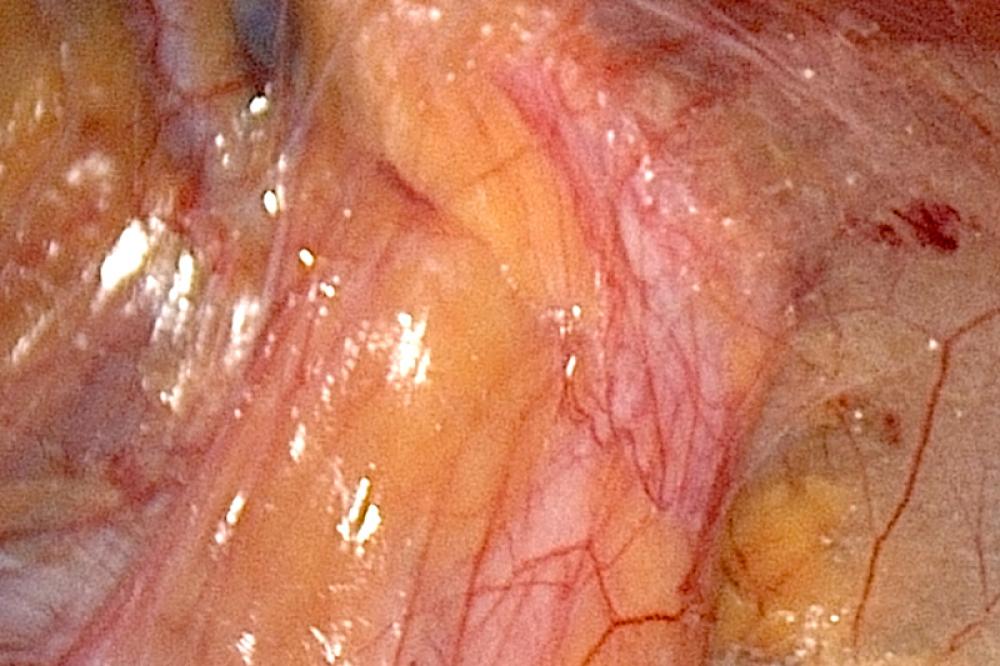
Genetics, aging, and previous surgery may contribute to a point of weakness in the layer surrounding your muscles that eventually turns into a hernia. A hernia might develop at a point of weakness caused by a previous surgical incision. A small out pouching that occurs months to years at a previous incision may be a sign of a hernia. Patients may witness a small soft balloon-like sac protrusion due to slackening of the muscular wall of the abdomen or at the site of the previous operation. These balloon-like protrusions may change in size according to position and may disappear when the abdominal wall is completely relaxed such as when you are lying down. This defect in the layer surrounding the muscles of your abdominal wall is called a ventral or incisional hernia. Sometimes, internal organs or a loop of the intestine may get trapped in this sac and cause a dangerous condition heralded by severe pain and discomfort.
Laparoscopic Ventral Hernia Repair Requires Mesh

This trapping of the intestines is called incarceration and can represent an emergency. Surgical interventions are often necessary to repair the defect in the abdominal wall and remove the sac-like protrusion. This operation is often performed using a small-telescope like instrument called a laparoscope.
Indications for laparoscopic repair
It is not always possible to carry out a laparoscopic ventral hernia repair. First and foremost, laparoscopic repair is only feasible if you are considered medically fit to undergo general anesthesia. Typically the next consideration is estimation on the part of the surgeon to surmise the amount of scar tissue that will be present inside the abdomen. Previous open incisions cause the intestine and other organs to be partially adherent to the underside of your abdominal wall. If you have many incisions or if your previous operation was for a very serious situation, the amount of scar tissue inside your abdomen might be estimated to be very high. In addition to this, surgery is feasible only if the surgeon is confident of the ability to place the laparoscopic trocars in positions that are deemed ergonomically feasible for their surgery. In some cases, the hernia may be so large that the abdominal wall gets so distorted that it proves to be difficult to safely place laparoscopic trocars.
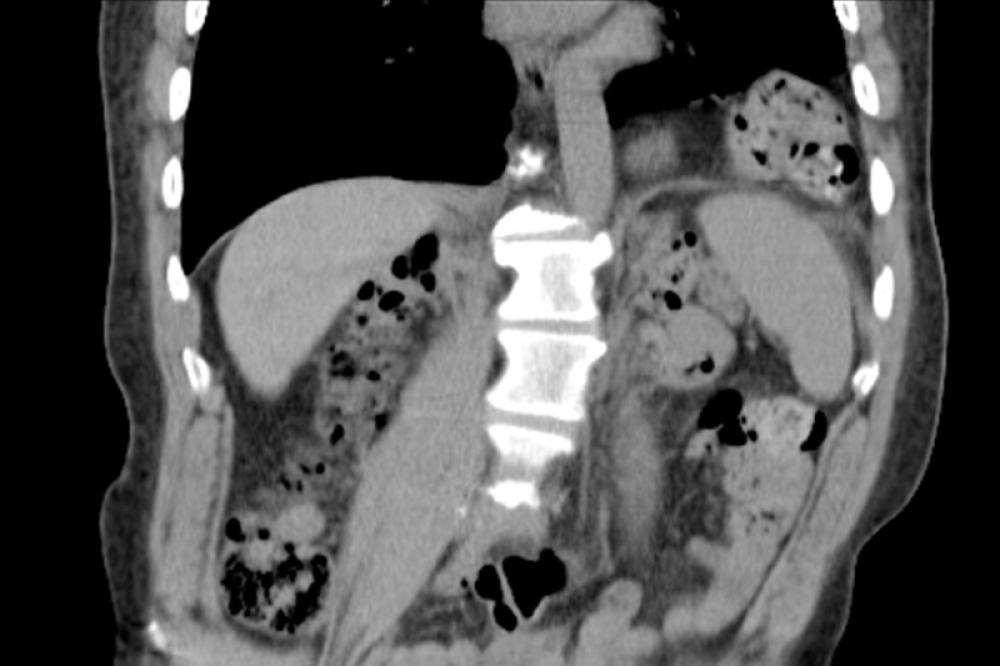
Multiple Defects

In some conditions, laparoscopic ventral hernia repair may not be feasible. The decision on whether a laparoscopic ventral hernia repair is feasible can be decided based on the physical examination, the number of previous incisions, as well as through ancillary studies such as a CT scan of the abdomen and pelvis. If you have a history of multiple operations and intrabdominal adhesions are suspected, you may be required to be on a clear liquid diet before your operation or you may need to have a special bowel preparation to evacuate the colon before surgery. These preparations help ensure that your intestines are empty and may also decrease the amount of intestinal bacteria in the colon.
Symptoms that prompt ventral hernia repair
With a ventral hernia, the you may find a bulge in the abdominal area, which is usually painless. However the hernia may be slightly tender and cause discomfort during physical strain like coughing and straining and during bowel movements. When the hernia becomes bothersome, you may consider having it repaired. One common finding is that the hernia bulge usually disappears when lying down and is more visible when standing. Other symptoms of hernia include vomiting, nausea and difficulty in having bowel movements. If there is continuous discomfort or nausea, it indicates that the hernia is strangulated and this is when the physician has to be contacted immediately.
The procedure
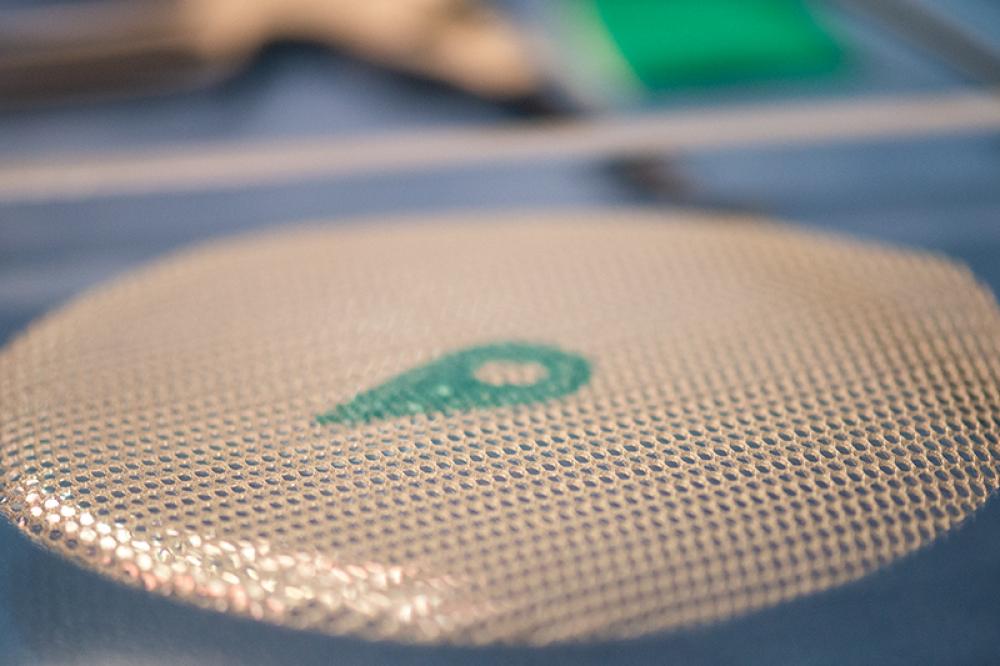
Ventral Mesh
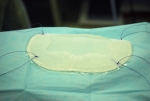
Special instruments, a videoscope, television monitors and small incisors are what are required for a laparoscopic ventral hernia repair. The surgeon first makes a small incision in the abdominal wall. It is up to the surgeon to choose the location where there is minimum risk of their running into organs and scar tissues that were involved in prior operations. A few other tiny incisions are made as required, depending on the amount of scar tissue that has to be removed, and how well they can see the hernia. Then a laparoscope is inserted through a small, hollow tube. It is through this laparoscope and TV camera that the surgeon can see the hernia in the body. Other instruments are then placed through a few more incisions to remove scar tissue in the body. With this, a surgical mesh is inserted into the abdomen, under the hernia defect, and attached to the surrounding stronger tissues found in the abdominal wall. This mesh is used to reinforce the weakened part of the abdominal wall, and thus prevent the hernia from recurring.
Advantages of laparoscopic ventral hernia repair
The greatest advantage of the laparoscopic ventral hernia repair when compared to the traditional surgical approach is that it offers quicker recovery with shorter hospital stays. In addition to this, there is a reduced risk of any infection and recurrence of the hernia. Patients usually return home within a day of the surgery, and have less pain with quicker return to normal activities.
Postoperative conditions
With laparoscopic ventral hernia repair, the chance of recurrence of hernia is about 10%, when compared to the 20 – 40% recurrence rate of the open procedure. Laparoscopic ventral hernia repair patients are generally encouraged to walk around as quickly as possible after the sugary. This is to avoid postoperative complications like pneumonia, pulmonary embolism and deep venous thrombosis. It is quite normal to experience some pain after the surgery wherein the patient is given IV narcotics as usual, and then put on oral analgesics the next day. After discharge, the patient has to visit the surgeon one to two weeks after discharge. No dietary restrictions have to be made after the operation while the amount of activity typically depends on a patient’s comfort level. However, it is not advised to engage in strenuous activities or heavy lifting for a few weeks, as the hernia mesh has to seal into place. When you experience fever, vomiting, chills, and difficulty in urinating and find some drainage from the incisions, call on the surgeon immediately. Otherwise, you can return to your normal activities within a short time of the surgery.