Robotic Heller Myotomy for Achalasia
Opening the Muscle

Achalasia means “failure to relax” and refers to a disorder of the muscle at the end of esophagus that doesn’t open normally during swallowing. It is also known as also known as esophageal achalasia, achalasia cardiae, cardiospasm, and esophageal aperistalsis. During achalasia, the smooth muscle that is responsible for swallowing looses its normal muscle tone and the lower esophageal sphincter does not relax correctly. Achalasia is a relatively rare condition with a prevalence estimated at less than 0.001%. A Laparoscopic or Robotic modified Heller myotomy is considered the standard of care for palliation of this incurable but benign disease.
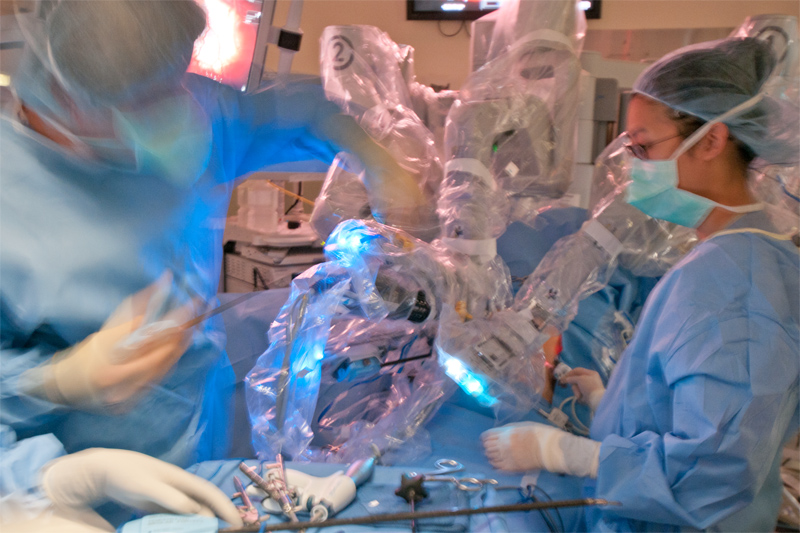
Combined Laparoscopic and Robotic Instrumentation

History
The description of the condition can be traced back to 1672 when Sir Thomas Willis performed a dilating procedure using a sponge attached to a whale bone. Ernest Heller performed the first successful esophagomyotomy almost 250 years later in 1913 and his name is commonly attached to the operation for achalasia- a “Heller Myotomy.” It wasn’t however until 1937 when F. C. Lendrum elucidated the mechanism of disease as the failure of the lower esophageal sphincter causing a functional esophageal obstruction.
What happens during achalasia?
The esophagus is a muscular tube that carries swallowed food from the back of the throat towards the stomach with a wave of contractions called peristalsis.
An antireflux procedure is tailored to the symptoms
Optimal Control
At the end of this muscular tube between the esophagus and the stomach, is a ring of muscle called the lower esophageal sphincter which encircles the esophagus below the diaphragm just above the entrance to the stomach. This sphincter muscle is normally contracted close to prevent the acidic stomach contents from refluxing backward into the esophagus known as gastroesophageal reflux or GERD. The act of swallowing causes a wave of esophageal contraction called peristalsis. Peristalsis pushes food along the esophagus. Normally, peristalsis causes the esophageal sphincter to relax and allow food into the stomach. In achalasia, which means "failure to relax," the esophageal sphincter remains partially closed. Normal peristalsis is interrupted and food cannot enter the stomach.
Different types of achalsia
Achalasia is a problem with the nerve cells that transmit messages to the esophageal musculature characterized by increased lower esophageal sphincter (LES) pressure, diminished or absent peristalsis in the distal portion of the esophagus composed of smooth muscle, and lack of a coordinated LES relaxation in response to swallowing. The ultimate cause of this degeneration is unknown. Autoimmune disease or hidden infection is suspected.
Leak Test
Primary achalasia is more common and is associated with a loss of ganglion cells in the esophageal myenteric plexus. These cells are inhibitory neurons responsible for esophageal sphincter relaxation and coordination of peristalsis. When these cells are gone, the sphincter can’t relax and peristalsis is not coordinated properly.
Secondary achalasia is less common and exists when a process affects the esophageal muscle cells in a manner different than the loss of ganglion cells. Secondary achalasia occurs with certain diseases such as Chagas disease (an infectious disease common in South America), diabetes mellitus, and some kinds of cancer.
Achalasia can be categorized by the diameter and length of the esophagus. An esophagus with a diameter less than 4 cm is grade 1, grade 2 is 4 to 6 cm, grade 3 is greater than 6 cm, and grade 4 is an enlarged twisted esophagus called a sigmoid esophagus.
What are the signs and symptoms of achalasia?
The Problem

Achalasia is characterized by difficulty swallowing, regurgitation, and sometimes chest pain. Difficulty in swallowing is called dysphagia and tends to become worse with time and involve the ability to swallow both solids and liquids. As this dysphagia becomes more advanced and the sphincter becomes less responsive, undigested food may be regurgitated and patients experience weight loss because of their difficulties with eating. Some achalasia patients also experience coughing when lying in a horizontal position and chest pain which may be perceived as heartburn. Retained food and liquid in the esophagus may accidentally go into the breathing tubes which is called aspiration. Aspirated food allows bacteria overgrowth in the lungs and causes a dangerous condition called aspiration pneumonia.
Tests and diagnosis
Due to the similarity of symptoms, achalasia can be mistaken for more common disorders such as gastroesophageal reflux disease (GERD), hiatal hernia, and even psychosomatic disorders.
Specific tests for achalasia are barium swallow and esophageal manometry. In addition, endoscopy of the esophagus, stomach and duodenum (esophagogastroduodenoscopy or EGD) is typically performed to evaluate any suspicious lesions and rule out the possibility of cancer.
Barium swallow
A barium swallow is sometimes called an esophagram or upper GI series. The test involves the patient swallowing a white chalk-like substance made of barium. This substance is carried down the esophagus just like any other fluid that is swallowed. A continuous series of xrays are performed (fluoroscopy) which allows a record of the peristalsis to be created. During achalasia, normal peristaltic movement of the esophagus is not seen. When the fluid gets to the lower esophageal sphincter, which does not relax properly, there is narrowing which produces a "bird's beak" appearance. The esophagus gradually stretches over time and varying degrees of a dilated esophagus may be seen.
Esophageal manometry
Manometry is also called an esophageal motility study. It is an outpatient test which requires a pressure sensor to be placed inside the esophagus. This sensor is contained in a thin tube which is inserted through the nose and passed into the esophagus. This sensor measures the pressure wave of the peristaltic contractions of the esophageal muscle with swallowing. This is a very sensitive test and considered one of the key tests for establishing the diagnosis of achalasia. Manometry in achalasia typically shows uncoordinated peristaltic contractions, increased intraesophageal pressure and failure of relaxation of the lower esophageal sphincter.
Medical and endoscopic treatment
Surgery is the preferred treatment for achalasia. Medications such as calcium channel blockers or nitroglycerin reduce the lower esophageal pressure but have limited utility. Botulinum toxin (Botox®) injected into the lower esophageal sphincter will paralyze the muscles that were not able to relax properly. The effect is temporary and lasts about 6 months but causes scarring in the sphincter which may increase the difficulty of later Heller myotomy. Pneumatic dilation uses forceful inflation of a balloon to stretch and tear the muscles of the esophageal sphincter. Each dilation caries a small risk of perforation and can causes increased scarring which may also make a Heller myotomy more difficult in the future.
Robotic Myotomy and fundoplication
Heller myotomy helps 90% of achalasia patients. Dr. Belsley uses a combination of laparoscopic and robotic instrumentation to perform the operation with small incisions. Preoperative testing will help determine the amount of dissection, use of bougie, extent of myotomy and need for an anti-reflux procedure.
Four or five small incisions are typically used. The liver retractor is inserted and the left lobe of the liver is elevated to allow identification of the gastroesophageal (GE) junction.The right and left crura of the diaphragm are identified as they extend into the mediastinum. Adhesions and the surrounding tissue of the esophagus are dissected proximally.
Transillumination
The thick muscle of the GE junction is divided up to the point where the muscle does not longer appear to be hypertrophic. This is typically located between 4 and 6 cm from the GE junction. The mucosa is identified and any small remaining fibers are divided. The myotomy is proximally complete when no remaining fibers are seen and the esophageal mucosa appears to bulge. The myotomy is then extended approximately two centimeters distal onto the stomach.
A Dor fundoplication is typically performed to protect the myotomy and prevent against reflux. The anterior part of the fundus is brought cephalad so that it lies over the myotomy. 2-0 Ethibond sutures are used to secure the fundus into position. Patients usually go home after one or two days in the hospital and are placed on a soft bland diet for several weeks to a month.
Lifestyle changes
Medical treatment, balloon dilatation and surgery provide varying degrees of palliation of symptoms. Both before and after treatment, achalasia patients need to eat slowly, chew well and drink plenty of water with meals. Avoiding eating at bedtime and raising the head of the bed helps prevents against reflux and promotes emptying of the esophagus by gravity. Proton pump inhibitors may be needed and foods that can aggravate reflux such as chocolate, mint, alcohol and caffeine may need to be avoided.
Follow-up
Even after successful treatment, swallowing may still become worse over time. The esophagus should be checked periodically with barium swallows as repeat treatments might be needed. Periodic endoscopy is also needed to check for reflux damage, which left untreated may lead to a premalignant condition known as Barrett's esophagus or a stricture.





