Why colon surgery is sometimes needed
The colon is the large intestine where the small intestine empties the metabolic wastes of digestion that are not absorbed in the body. After absorption of water, the colon expels these wastes as faeces through the rectum at regular intervals. Common colon ailments include irregular bowel movements, growth of polyps, and colon cancer. Sometimes, surgical interventions are necessary to take care of these problems in the colon. As people grow older, often small outpouchings of the intestine form called colonic diverticuli. Diverticulosis and diverticulitis are conditions that arise from these outpouchings of the intestine and may sometimes cause bleeding and infection. If you have suffered multiple attacks then you may require an operation to remove the effected portion of the colon.
Cancer may sometimes develop in the colon therefore colonoscopy is a very valuable diagnostic tool and every patient should have a colonoscopy by age 50. The doctor will typically perform a biopsy if a polyp is seen in the colon and this will help decide whether surgery is indicated. Sometimes a suspicious looking intestinal polyp may be seen on colonoscopy which is too large or in too difficult a location for the endoscopist (your GI doctor) to remove. If colonoscopy is not indicated because of severe diverticulosis or the question of an obstruction or blockage, then a barium enema is another test which surgeons can use to look inside the colon and help them to decide on surgery. Sometimes, a CT scan of the abdomen may be a useful tool to decide if a colon surgery is needed. Laparoscopic colon surgery is a minimally invasive surgical procedure with which the surgeon can take out portions of the colon using a few small incisions.A CT scan may help provide information to help plan port placement and the approach for the operation. Many different procedures can be performed and therefore many factors determine the optimal procedure and time to return to normal activities.
Advantages of Laparoscopic colon surgery
The greatest advantage of a laparoscopic colon surgery over an open surgery is that it offers less postoperative pain, a shorter hospital stay and permits the patient to return faster to a solid food diet. With this, there is a quicker return to bowel functioning, improved cosmetic results and faster return to normal activities.
Preparing for surgery
Prior to the laparoscopic colon surgery, you have to have had a complete medical work-up by your medical doctor and gastroenterologist. Just prior to the operation, the colon and rectum is emptied before surgery by drinking special cleansing solutions. The patient has to be on a diet of clear liquids, laxatives and enemas one day before the operation to ensure the colon is completely empty before surgery. If this is not completed, it is unsafe to undergo the operation. So, if you find any discomfort in taking the preparations, the surgeon has to be contacted to reschedule the surgery. No food or liquids, besides medications that you have discussed with the surgeon should be taken after midnight prior to the operation. Drugs like aspirins, anti-inflammatory medicine, blood thinners and vitamin E has to be stopped a week before surgery. Some homeopathic medications including, diet medication and St. Johns Wort must also be stopped for two weeks before surgery.
The procedure
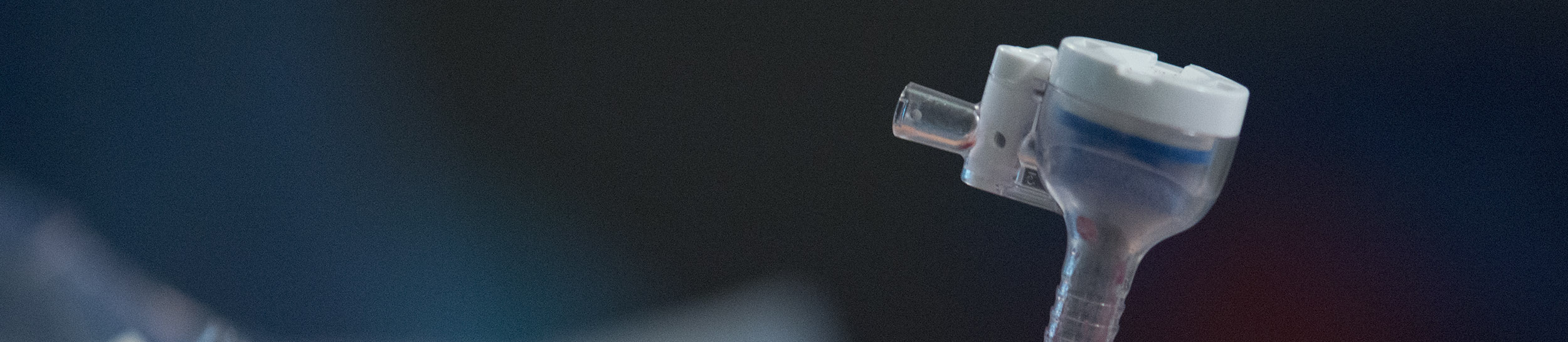
The surgeon makes small incisions on the abdominal wall to allow laparoscopic colon surgery. Then the surgeon enters the abdomen using a narrow tube-like instrument called cannula, through which a laparoscope is inserted. This gives the surgeon a magnified view of the internal organs of the patient, on a television monitor. Then a few other cannulas are inserted so that the surgeon can work inside, to remove parts of the colon. The surgeon can complete the complete procedure through all these cannulas. The diseased portion of the colon will be taken out of the body by lengthening one of these small cannula incisions.
When laparoscopic colon surgery is not feasible.
It is sometimes not feasible to conduct laparoscopic colon surgery on very obese patients, those with large large tumors in the colon, and those in which the doctor finds it difficult to visualize internal organs. Those patients who already have a history of abdominal surgery with dense scar tissue and those who experience bleeding problems during the operation may require that the surgeon perform an open surgery to complete the procedure. It is left to the surgeon to decide on the feasibility of the surgery on the patient before or during the operation. And if the surgeon decides to convert to open procedure, it does not indicate a complication in the surgery; but more of a sound judgment on the part of the surgeon.
Postoperative care
The doctor encourages you to get out of bed a day after laparoscopic colon surgery, and to start walking. This is to encourage deep breathing and prevent a condition called atelectasis. Patients typically spend between two and four days in the hospital after colon surgery depending on the indication for the procedure and which portion of the colon was removed. Usually, patients can return to normal activities in one to two weeks time. These normal activities include showering, walking up stairs, and performing light work. You will of course, have to visit the surgeon for a follow-up appointment within 2 weeks of the operation.
Risks associated with laparoscopic colon surgery:
Like any form of surgery, there is a possibility of some complications arising with laparoscopic colon surgery. These complications include bleeding and infection at the site of the operation. Some patients may find a leak at the point the colon was connected together or blood clots in the lungs. There are also patients who find injury to adjacent organs like ureter and bladder. Early recognition of these possible conditions is important so that the right course of action can be decided. However, if there is any fever, abdominal pain, chills or rectal bleeding, the surgeon has to be contacted immediately. The surgeon also has to be contacted immediately if you find some increased abdominal swelling, persistent nausea, pain that cannot be relieved by pain medications and a persistent cough or shortness of breath. Even purulent drainage from any of the incisions of the surgery, and redness around the incisions that worsens or grows bigger has to be informed to the surgeon. Although like any surgery on the intestines, intestinal function will be changed for a few weeks after the operation. If however you find it very difficult to eat or drink liquids, contact the doctor immediately.